How Data Science Is Ending the Era of One Size Fits All Therapy for Depression
A new perspective on depression: how targeting specific subtypes will deliver better outcomes
Executive summary
Precision medicine for many physical conditions has been available for a number of years, with tailored treatments that target different types of cancer and diabetes, for example. This is not the case for mental health disorders, largely because their underlying complexity and diversity has not yet been fully explored.
Depression, for instance, can present in a distinct way from one patient to another. Patients with the same severity of depression may have very different symptoms. However, current methods for diagnosing and treating the condition are unable to capture these nuances.
If the specific subtypes of mental health conditions can be identified, therapy for each patient can be personalised to their individual symptoms. In addition to enabling more accurate diagnosis, precision medicine in mental healthcare will increase the effectiveness of treatment and quality of care, and therefore the likelihood that the patient will recover.
Ground-breaking research completed by ieso, in partnership with the University of Sheffield, has identified five broad subtypes of depression, along with 14 depressive states characterised by distinct symptom profiles. Through mining and analysing rich data sets collected from ieso and healthcare trusts across England, the team has also been able to determine how each subtype responds to treatment.
This study is the first to demonstrate conclusive evidence of the existence of different dimensions and subtypes in depressive symptoms. Their discoveries have laid the foundations for changing the way we characterise and treat depression, significantly improving outcomes for patients, and driving efficiencies for service providers.
The era of one-size-fits-all therapy for depression is over.
Introduction
Depression can be a very debilitating condition, and it can present in a very different way from one individual to another. Some patients might feel very tired or low in energy, have trouble sleeping, and experience changes in appetite. Others will show symptoms around low self-esteem or negative thinking patterns.
Current methods for diagnosing and treating depression are not built to capture the full scope of symptoms, their unique combinations and characteristics, and their variability. Nor has it historically been clear how different depressive symptoms respond to treatment.
Studies undertaken by ieso, in partnership with the University of Sheffield, have resulted in a breakthrough that lays the foundation for precision treatments for depression that are tailored to a patient’s symptoms. The research has led to the discovery of five distinct subtypes and 14 different states of depression, along with unique insights into how they respond to treatment and evolve over time. These findings have the potential to significantly improve outcomes for patients, and drive efficiencies for service providers.
Insufficiencies in knowledge
Many studies have examined various mental health conditions in depth, including depression, and these have suggested the existence of different subtypes of depression. However, they failed to analyse the variability of characteristics within depressive symptoms. This has largely been due to a lack of data and analytical tools capable of examining large samples.
The insights that emerged from these studies have never been incorporated into diagnostic systems either. As a result, these systems have failed to capture the underlying complexity of mental health disorders.
Defining what constitutes each depression subtype has also been difficult historically. In combination with lack of consistent terminology and criteria around symptoms, this has led to a lack of progress in treatment that targets specific types of depression.
Another issue is the lack of objective and systematic methods for measuring the impact on different subtypes of delivery of psychotherapy.
According to the World Health Organisation (WHO), the global burden of depression is on the rise and is a leading cause and contributor to disability and disease. Data published by the organisation in 2018 estimated that around 264 million people of all ages were suffering from the condition.
A sharp rise in mental ill health
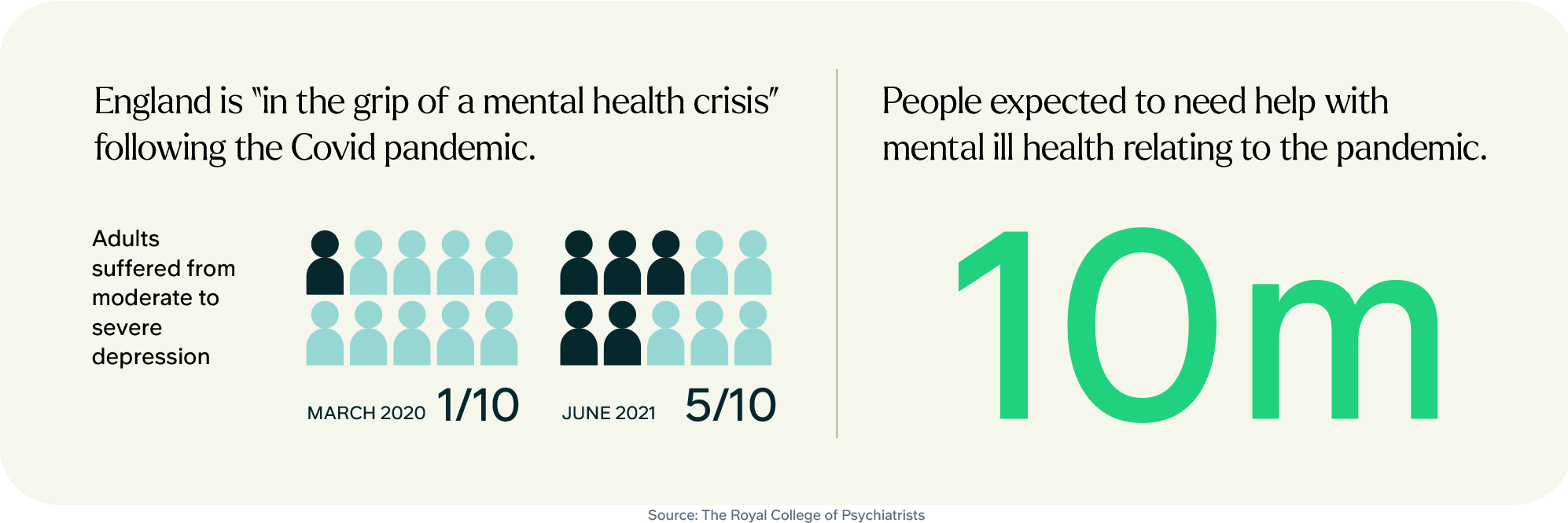
Mental health services in the UK are under enormous pressure. Analysis of NHS (National Health System) and Office for National Statistics data by the Royal College of Psychiatrists indicates that England is “in the grip of a mental health crisis” following the Covid pandemic. Until March 2020 about one in 10 adults suffered from moderate to severe depression, but that had doubled to almost one in five by last June. Around 10 million people are expected to need help with mental ill health relating to the pandemic.
This increased pressure presents significant strategic challenges to mental health services. They are required to deliver meaningful outcomes for the person seeking help (ref), but the current rate of improvement is poor(ref). Despite the wide range of treatments available, from various types of therapy to pharmacological interventions, only half of patients recover (ref1) (ref2).
“(The) data from the Office for National Statistics, which reveals that depression rates have doubled since the COVID-19 pandemic began, forewarns of a growing mental health crisis in the UK… Despite increasing rates of depression, diagnoses by GPs (General Practitioner) fell by almost a quarter, suggesting access to mental health care is in decline. Our COVID-19 impact inquiry has found that reduced access to care will have long-term implications on mental health and put even greater pressure on health services.”
Jo Bibby, Director of Health, the Health Foundation
Introducing precision treatments for mental health conditions, that are targeted to a patient’s specific symptoms and subtype, will drive a major shift in quality of care, making diagnosis more accurate and increasing likelihood of recovery. Taking a more personalised approach to treatment planning has become the norm in medicine, and it is time for the same approach to be introduced into mental healthcare.
Capturing the nuances of mental illness
Data and clinical evidence hold the key to progress in mental health for patients, clinicians, and the community at large. Three research studies undertaken by a team at ieso, collaborating with scientists from the University of Sheffield, have led to a breakthrough into new ways of identifying depression subtypes and treating depression.
ieso has a rich data set drawn from hundreds of thousands of hours of anonymised therapy transcripts, from which it is learning more and more about conditions, causes, symptoms, treatments, and even prevention. Applying AI (Artificial Intelligence) and deep learning to this data has enabled the researchers to pinpoint patterns, and identify which contents of psychotherapy are significantly associated with positive clinical outcomes (ref). These technologies also make it possible to analyse large clinical data sets.
The ieso and University of Sheffield team analysed this data with the aim of identifying distinct states and subtypes of depression, alongside large-scale independent data sets collected from healthcare trusts across England spanning almost 10 years. They were then able to consistently replicate the results in three separate experiments.
Their work is the first to look at different depression states in a real-world clinical setting, and their response to cognitive behavioural therapy (CBT). It is also the first study to isolate depression states in a large sample in order to characterise transitions between those states, and to analyse how they respond to highly standardised evidence-based psychological treatments. The study also revisited the classification system for determining the best treatment for a particular patient.
The 14 depressive states
According to the results, depression is a condition that is diverse in content. The studies identified 14 depressive states with distinct symptom profiles, which were classed into three categories:
- Cognitive depression – low self-esteem, negative thinking patterns, low mood
- Affective depression – inability to feel pleasure, lack of motivation, burnout
- Somatic/physical depression – tiredness, difficulty sleeping and loss of appetite
These states were then clustered within five broad subtypes of depression: mild, severe, cognitive-affective, somatic, and typical.
The five subtypes of depression
Mild: Minimal symptoms, a state of mild overall severity (2.7% of patients).
Severe: A serious state of depression, people typically experience all symptoms at a very elevated level (9.8% of patients).
Cognitive-affective: Intense feelings of depression, tiredness, and low self-esteem. People may have repetitive negative thoughts and struggle to feel pleasure in activities they usually enjoy and lack motivation (23.7% of patients).
Somatic: Difficulties sleeping, feeling of tiredness and changes in appetite, as well as psychomotor disturbances such as restlessness, fidgeting and pacing (21.4% of patients).
Typical: Patients experience a combination of both cognitive-affective and somatic symptoms to varying degrees of severity (42.4% of patients).
Whereas depression has typically been considered as biochemical-based or emotionally-rooted, the analysis shows that there is often a physiological element to patients’ symptoms.
Transitions between states and subtypes
These subtypes are stable over time: they are likely to change in severity but are less likely to transition into other subtypes. In other words, while patients can move through depressive states, they remain within the same subtype, even as their symptoms decrease in severity over a course of treatment. The most common transitions recorded were from severe towards milder states, within the same depressive subtype.
The different subtypes also show distinct engagement and response patterns with regards to treatment.
The effectiveness of CBT
The hypothesis for distinct depressive profiles, and differences in the probability of a patient transitioning across depressive states, was further scrutinised by looking at how each subtype responds to CBT.
Rates of engagement with therapy varied. When treated with CBT, patients in somatic and typical states were found to have significantly lower rates of engagement than those in cognitive-affective states. For instance, somatic patients attended fewer sessions, and their condition improved less reliably. Patients with a typical subtype were more likely to drop out of treatment compared to those with cognitive‐affective and somatic subtypes. On the other hand, the cognitive-affective and most severe subtypes registered the highest improvement rate.
Methodology
ieso and University of Sheffield research team analysed the type and severity of symptoms of more than 8,000 patients experiencing depression.
Latent transition analysis was applied to a large (N = 8380) multi-service sample of patients treated with CBT in outpatient clinics. Patients were classed into initial latent states based on their responses to the Patient Health Questionnaire-9 of depression symptoms, and transition probabilities to other states during treatment were quantified. Qualitatively similar states were clustered into overarching depression subtypes, and the team statistically compared indices of treatment engagement and outcomes between subtypes using post hoc analyses.
Demographic differences
The research team also examined patient demographics across depressive states. Patients in somatic subtypes were more likely to be female, with long‐term physical health conditions, who were taking prescribed pharmacotherapy. In fact, one of the most significant features characterising the somatic depression subtype is the presence of long-term health problems.
Males were more likely to have the cognitive-affective subtype of depression. Of those patients that exhibited high levels of suicidal risk, females were more likely to have the cognitive-affective subtype and males were more likely to have the typical subtype.
“Given how different depression can be from one person to the next, a treatment that works for one person may not work as well for another. Our findings have helped to identify how symptom profiles can be grouped into replicable subtypes of depression, showing that not all patients respond to CBT treatment in the same way.”
Dr Melanie Simmonds-Buckley, University of Sheffield
The dawn of tailored treatments
ieso’s studies are the first to demonstrate conclusive evidence of the existence of distinct dimensions or subtypes of depressive symptoms. This evidence has the potential to give rise to a new generation of personalised treatment planning for depression, which treats symptoms and severity rather than severity alone. If the insights gained are used to enable more precise assessment of patients, and to develop interventions that address specific depressive states and treatments, the chances of positive outcomes will be much higher.
Patients with the same overall severity of depression may present with distinct symptoms and contributing factors. They will therefore require a different type of therapy, with change methods and active ingredients tailored specifically to their symptom profile.
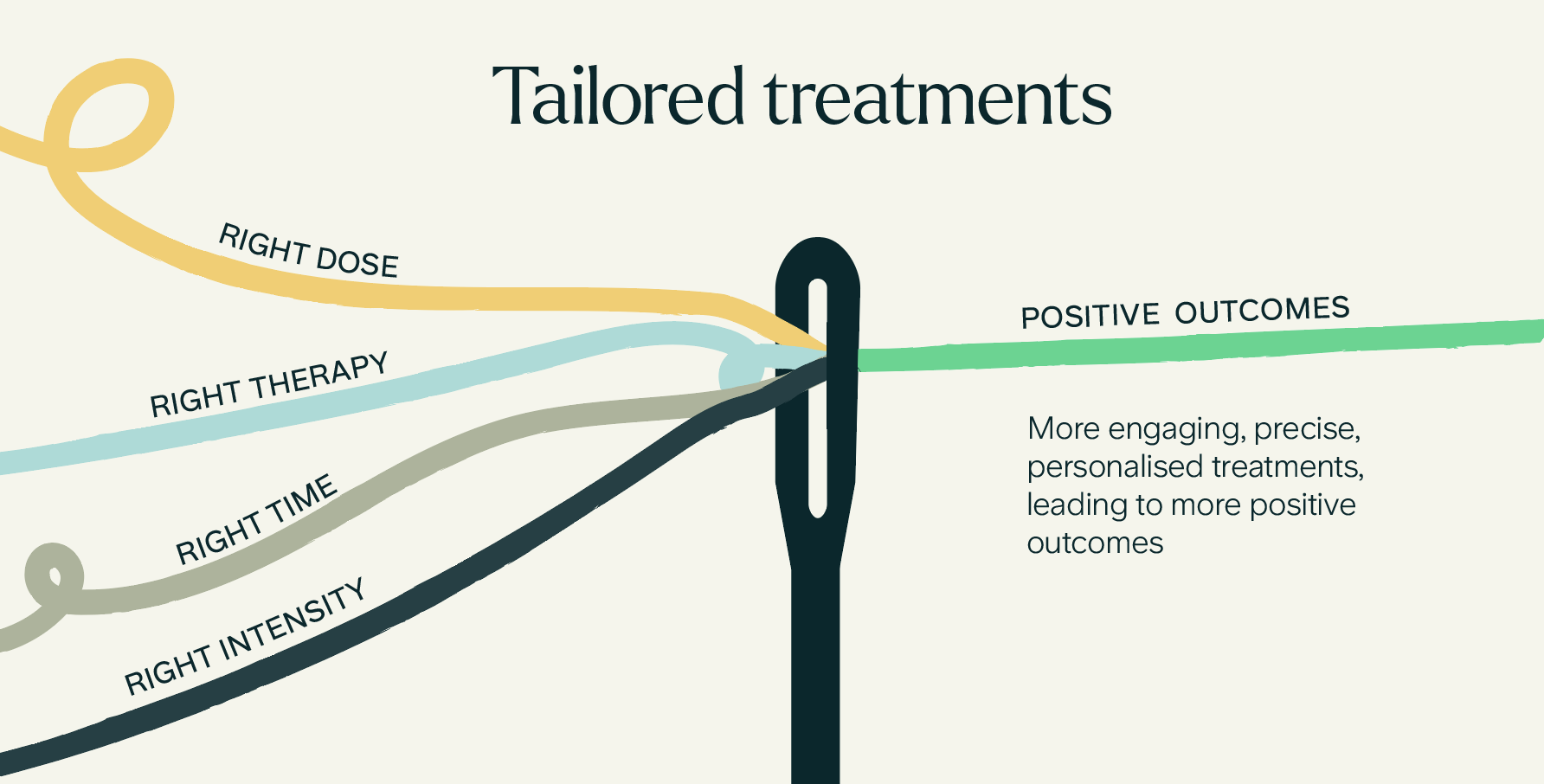
Knowing which patient and service variables are linked to positive clinical outcomes can be used to develop targeted treatment protocols. Giving patients the right dose of the right therapy at the right time at the right intensity will lead to higher engagement, and increase the likelihood of positive outcomes (ref). Care will also become more cost-effective for mental health services providers due to more efficient treatments, and the reduced likelihood of recurrence.
The discoveries made also enable the development of specific measurement criteria that are consistent across all depressive profiles, regardless of severity, leading to more precise monitoring of treatment effectiveness and progress to recovery.
The studies provide insight into how different types of depression evolve over time, and how they respond to treatment. It is evident that symptom severity and profiles can, and will, change over a course of therapy.
Depression symptoms can involve the body, as well as the brain. Based on the evidence from the study it could be hypothesised that people who are more likely to develop depression with somatic features share underlying physiological traits and are likely to be females who are living with long-term physical conditions. They don’t respond as well to CBT as other subtypes, which could lead to other types of treatments being prioritised for patients with this subtype.
Enabling early intervention
Prevention and early intervention lead to higher likelihood of recovery (ref). The insights gained from ieso’s studies make it possible to determine at the triage stage what depression subtype a patient may be in, and this knowledge can inform the best treatment pathway. Prioritising allocation of patients with severe and somatic depression for example, who are less likely to respond, could lead to improved outcomes for these individuals.
The method of subtyping used by ieso could potentially be implemented as part of a digital triage tool, to identify patients in one of the depressive states that respond least positively to treatment. Those at higher risk of dropout, and with a lower chance of symptomatic improvement, could then be prioritised for clinical supervision.
The findings could also be used to detect the onset of ill mental health, by being incorporated into mood and symptom checkers, like this one, which can help individuals spot the early symptoms of poor mental wellbeing and provide suggestions on how to cope.
Driving up recovery across mental healthcare
The new more specific and rigorous perspective on depression presented by ieso’s research opens up exciting possibilities for future exploration and hypothesis. Will depression become easier to treat? Which specific change methods work best – for instance, cognitive vs behavioural? With evidence that depression has a physiological as well as emotional component, will mental health carry less stigma? Will doctors look at it through a medical lens, with more specificity and clarity?
It also lays the foundation for further research into new types of therapies, their components, and the determinants of effectiveness and recovery.
The collective evidence offered by the ieso and NHS data sets analysed in these studies also has huge potential to help drive up standards right across mental healthcare, by shedding new light on how to improve outcomes for people with other mental health conditions, such as anxiety.
Within this data lie the insights needed to drive innovation in the mental healthcare arena, help service providers and government identify where they need to act, assist in the benchmarking and evaluation of services, assess the effectiveness of psychotherapy, and monitor the patient and therapist experience (ref.)
Read more
Researchers conducted a study with 299 UK participants to evaluate if the digital program was acceptable and engaging, and if it was safe & effective in improving symptoms of anxiety, worry or stress.
In this team spotlight interview, we spoke to Brendon Kelly about his role as Head of US Business Development.
Researchers conducted a study to understand if patients who used the ieso Digital Program for anxiety found it acceptable, engaging, and usable.

